With early diagnosis and correct medication and treatment, glaucoma can be controlled. However, sight loss resulting from glaucoma cannot be restored. At the present time, there is no cure. Once detected, glaucoma usually requires ongoing, long-term care. Keeping your eye pressure under control is very important. You must follow your treatment plan carefully to help control your eye pressure. This will protect the optic nerve and prevent sight loss.
Many people think that glaucoma has been cured when high eye pressure is lowered to safe levels with medication or surgery. In fact, the glaucoma is only being controlled, not cured. Regular check ups are still needed even after medications or surgeries have controlled the eye pressure.
Target pressure
The eye specialist will decide which range of pressure is acceptable for each individual case, in order to maintain vision and avoid progression. The target pressure is decided based on the severity of glaucoma, the age of the patient, corneal thickness etc.
Glaucoma Medications 
Glaucoma is typically treated with the use of medications that either help increase fluid drainage or decrease fluid production by the eye. In most cases, medication can safely control eye pressure for many years.
Laser treatment
There are several types of laser surgery used to treat glaucoma. The type of laser surgery will depend on the form of glaucoma and how severe it is. Laser surgeries are performed in an outpatient setting in your doctor’s office or at the clinic.
Laser surgery is the main initial treatment method for angle-closure glaucoma, which results in widening of the angle for most patients. In cases of open-angle glaucoma, laser surgery can be used as an adjunct treatment with medications.
Incisional Surgery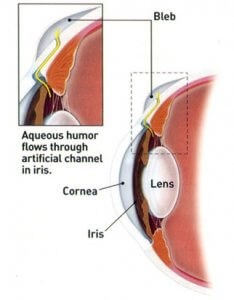
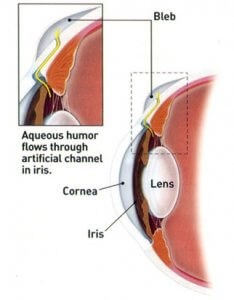
Incisional surgery is usually considered when the maximum amount of medication is not controlling your eye pressure or when your glaucoma is progressing despite normal pressures.
What happens during surgery is that a new drainage is opened for the fluid to drain and the eye to maintain low pressures. The most common types of surgery is trabeculectomy, where the drainage channel is made from the patients own tissues, and tube surgery, where an artificial valve or tube is placed in the eye so that the fluid can drain.
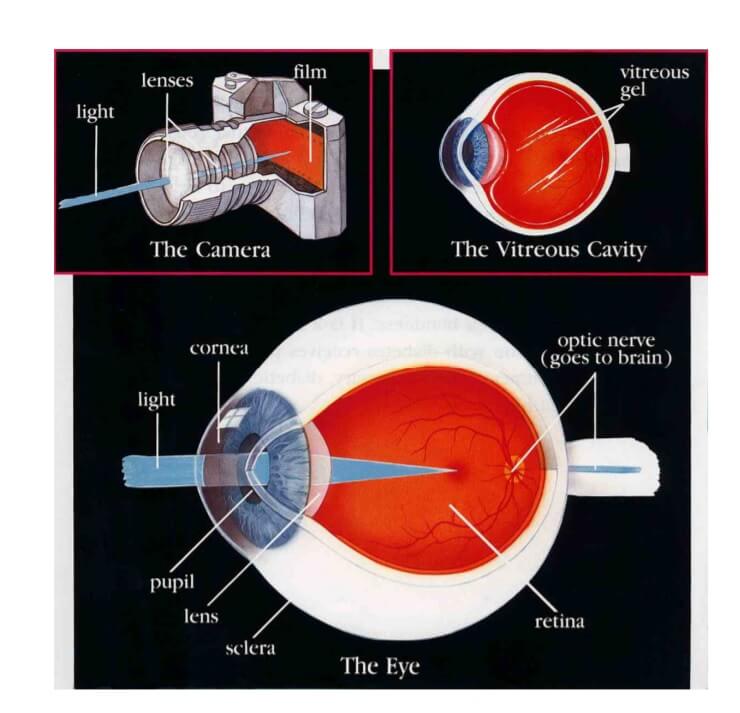 vers the back inside wall of the camera. When the light hits the film, a picture is taken. The eye works in much the same way. The front parts of the eye (the cornea, pupil, and lens) are clear and allow light to pass through. The light also passes through the large space in the centre of the eye called the vitreous cavity.
vers the back inside wall of the camera. When the light hits the film, a picture is taken. The eye works in much the same way. The front parts of the eye (the cornea, pupil, and lens) are clear and allow light to pass through. The light also passes through the large space in the centre of the eye called the vitreous cavity. The
The 










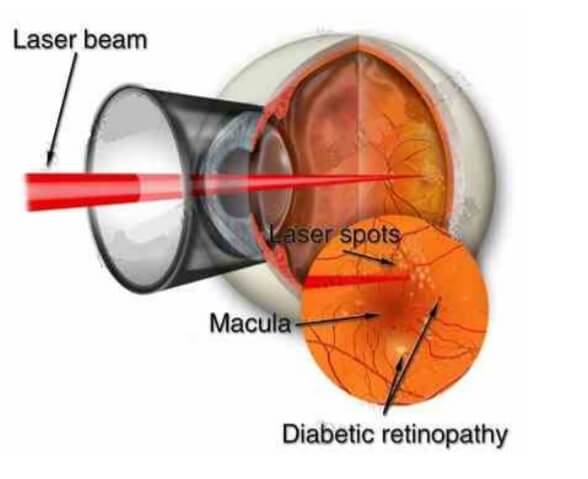 very helpful for the treatment of diabetic retinopathy. The laser beam is a high energy light that turns to heat when it is focused on the parts of the retina to be treated. The laser heat seals the leaking blood vessels of the macula and reduces their leakage. Essentially, the major purpose of laser surgery is to prevent further visual loss. Vision is not often improved by laser and it may even be reduced by laser treatment, especially in the initial stages. If however laser treatment is not performed when it becomes necessary then visual deterioration will usually progress rapidly.
very helpful for the treatment of diabetic retinopathy. The laser beam is a high energy light that turns to heat when it is focused on the parts of the retina to be treated. The laser heat seals the leaking blood vessels of the macula and reduces their leakage. Essentially, the major purpose of laser surgery is to prevent further visual loss. Vision is not often improved by laser and it may even be reduced by laser treatment, especially in the initial stages. If however laser treatment is not performed when it becomes necessary then visual deterioration will usually progress rapidly.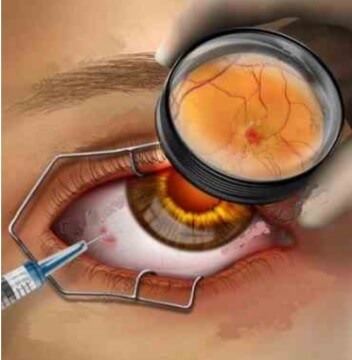 ugs (antiVEGFs). Injection of an anti-VEGF drug into the vitreous cavity is used to reduce macular oedema (fluid at the back of the eye) and reduce new vessel growth. The injection is administered after the instillation of anaesthetic drops onto the eye which renders the procedure painless. The sterile environment of an operating theatre is used to minimize the risk of infection.
ugs (antiVEGFs). Injection of an anti-VEGF drug into the vitreous cavity is used to reduce macular oedema (fluid at the back of the eye) and reduce new vessel growth. The injection is administered after the instillation of anaesthetic drops onto the eye which renders the procedure painless. The sterile environment of an operating theatre is used to minimize the risk of infection.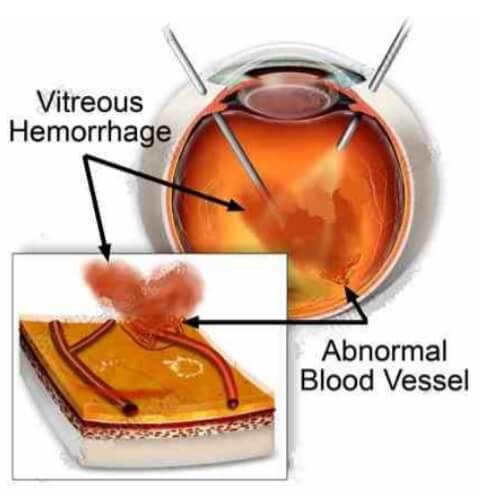 When a person does notice the sudden appearance of floaters, spider webs, spots in front of the eyes, or blurred vision, they should immediately call their eye doctor. Usually these are symptoms of a vitreous haemorrhage. If there is so much vitreous haemorrhage that laser surgery is not possible, or if the blood does not disappear on its own, it can be removed with an operation called a vitrectomy. Vitrectomy surgery is done in the hospital, under general or local anaesthesia. The blood-filled vitreous gel is removed. It is replaced during the operation with a gas bubble or a clear fluid that is compatible with the eye. Over time, the gas bubble or fluid is absorbed by the eye and is replaced by the eye’s own fluid.
When a person does notice the sudden appearance of floaters, spider webs, spots in front of the eyes, or blurred vision, they should immediately call their eye doctor. Usually these are symptoms of a vitreous haemorrhage. If there is so much vitreous haemorrhage that laser surgery is not possible, or if the blood does not disappear on its own, it can be removed with an operation called a vitrectomy. Vitrectomy surgery is done in the hospital, under general or local anaesthesia. The blood-filled vitreous gel is removed. It is replaced during the operation with a gas bubble or a clear fluid that is compatible with the eye. Over time, the gas bubble or fluid is absorbed by the eye and is replaced by the eye’s own fluid.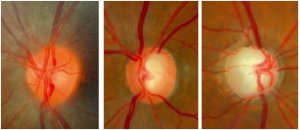
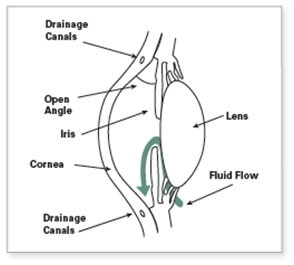
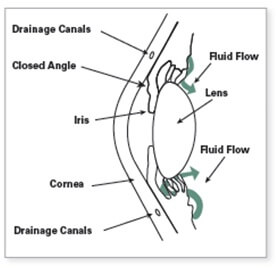 In this type, the angle is closed in many or most areas. This rise in eye pressure may occur suddenly (an acute attack of angle closure) or gradually. If the intraocular pressure rises very quickly, it causes symptoms such as eye pain, blurry vision, redness, rainbow colored rings (or haloes) around lights, and nausea and/or vomiting. An acute attack of angle-closure glaucoma can cause permanent vision damage and requires immediate medical attention. The gradual form of angle-closure (chronic angle-closure glaucoma) usually has no symptoms and may not be apparent in the earlier stages without an eye examination.
In this type, the angle is closed in many or most areas. This rise in eye pressure may occur suddenly (an acute attack of angle closure) or gradually. If the intraocular pressure rises very quickly, it causes symptoms such as eye pain, blurry vision, redness, rainbow colored rings (or haloes) around lights, and nausea and/or vomiting. An acute attack of angle-closure glaucoma can cause permanent vision damage and requires immediate medical attention. The gradual form of angle-closure (chronic angle-closure glaucoma) usually has no symptoms and may not be apparent in the earlier stages without an eye examination.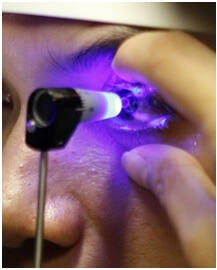
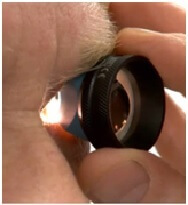 Gonioscopy is a diagnostic exam that helps determine whether the angle formed by the iris and the cornea is open and wide or narrow and closed. During the exam, eye drops are used to numb the eye and a special hand-held contact lens is gently placed on the eye for a few moments.
Gonioscopy is a diagnostic exam that helps determine whether the angle formed by the iris and the cornea is open and wide or narrow and closed. During the exam, eye drops are used to numb the eye and a special hand-held contact lens is gently placed on the eye for a few moments.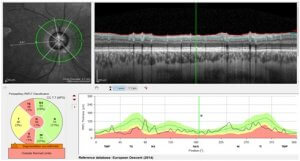

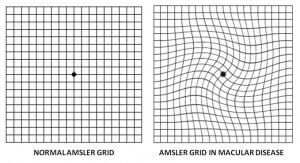 There is no substitute for regular eye examinations with your eye doctor, but there is a way to check for vision symptoms at home. To test your vision for AMD, use a checkered square known as the Amsler grid.
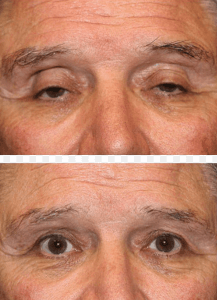
There is no substitute for regular eye examinations with your eye doctor, but there is a way to check for vision symptoms at home. To test your vision for AMD, use a checkered square known as the Amsler grid.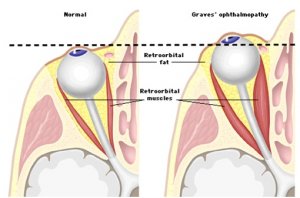 Thyroid eye disease (TED), also known as Graves’ disease, is an autoimmune inflammatory disorder affecting the tissues within the eye socket. It can cause pain, swelling, redness, watering, retraction of the upper eyelids giving a staring appearance, bulging eyes, double vision and occasionally decreased vision.
Thyroid eye disease (TED), also known as Graves’ disease, is an autoimmune inflammatory disorder affecting the tissues within the eye socket. It can cause pain, swelling, redness, watering, retraction of the upper eyelids giving a staring appearance, bulging eyes, double vision and occasionally decreased vision.