The doctors have put together some information for your reference .
Eye Operations
Eye Operations
- What is a cataract and how is it removed
The eye is like a camera. When you take a picture, the lens in the front of the camera allows light through and focuses that light on the film that covers the back inside wall of the camera. When the light hits the film, a picture is taken.
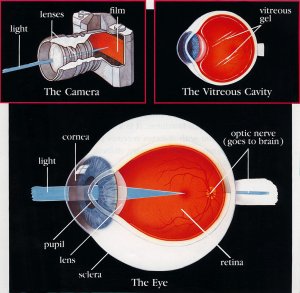
The eye works in much the same way. The front parts of the eye (the cornea, pupil, and lens) are clear and allow light to pass through. The light is focused by the cornea and the lens onto a thin layer of tissue called the retina, which covers the back inside wall of the eye. The retina is like the film in a camera. It is the seeing tissue of the eye. When the focused light hits the retina, a picture is taken. Messages about this picture are sent to the brain through the optic nerve. This is how we see.
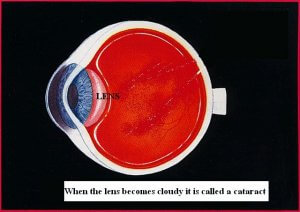
When the lens of the eye becomes cloudy or opaque it no longer allows light to enter the eye and the vision deteriorates. An opaque or cloudy lens is called a cataract. This is what needs to be removed and replaced in order to restore vision
- Instructions for Cataract surgery under local anaesthetic
Your cataract will be removed completely painless using the technology of laser (FLACS-Femtosecond Laser Assisted Cataract Surgery with use of LenSx-ALCON) and ultrasound (Phacoemulsification with Centurion-ALCON) to liquefy and aspirate the cataract. A foldable lens implant is then inserted into the eye and usually sutures are not required.
You will be able to go home immediately after the operation is completed.
It is very important therefore to follow your postoperative instructions carefully.
- On the day of surgery have a light breakfast and if you have been prescribed drops to use prior to surgery do so as instructed.
- You can come dressed in your normal clothing. There is no need to bring any nightclothes with you. You will be taken to the operating theatre by the nursing staff when its time for your surgery, this is usually between 1 to 3 hours after your arrival depending on the preparation time necessary and how busy the theatre timetable is on that day.
- In the operating theatre you will receive some local anaesthetic drops 15 to 20 minutes before your surgery. Usually an injectable local anaesthetic is not necessary, if it is this will be explained to you. During the operation you will be wide-awake and you will be able to hear everything but you will not see or feel any part of the operation. You will be able to talk to the surgeon at any time and tell him if you have a problem. At the end of the procedure your eye will be closed with an eye pad and you will go home.
- During your first evening after the surgery feel free to do as you please as long as you keep your eye pad dry and intact. If you develop a headache you can take your normal pain relief that you would use at any other time.
- The following day you will need to attend for a post operative visit as instructed and have your eye pad removed. Your eye will remain open from then on. You will have good vision from day one but will continue to improve for about one month. You will then be examined again and told if you need to go to your optician for new glasses.
- Refractive surgery
Refractive surgery is the operation using laser technology (excimer laser) to change the refractive status of the eye.
It has become one of the most popular procedures in medicine and since 1983 over 20 million such procedures have been performed worldwide.
What are the benefits?
Reduce or eliminate dependence on glasses, improve appearance and give the ability to play sports unhindered
Is the procedure effective and permanent?
One year after treatment over 95% of people with low to moderate prescriptions are able to pass a driver’s license vision test without corrective lenses.
How the excimer laser works?
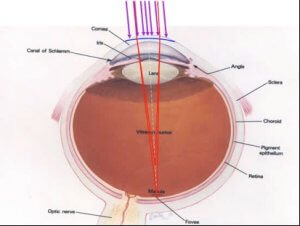
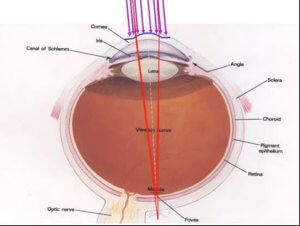
It uses a cool ultraviolet beam to precisely remove (ablate) very tiny bits of tissue from the surface of the cornea in order to reshape it. When you reshape the cornea in the right way it focuses light into the eye and onto the retina, providing clearer vision than before.
Criteria for good results
– Over 21years old
– Stable refraction for at least 12 – 24 months
– No other eye problems
– Good general health
– Realistic expectations
What methods of refractive surgery exist?
LASIK
During the procedure a thin-hinged flap is created by a laser (femtosecond). The flap is lifted and then laser energy is applied underneath to reshape the eye. The flap is replaced and functions as a natural bandage.
“The surgery takes a few minutes, is done with the use of local anesthetic drops and the person returns fully to the activities of the after 2-3 days”

PRK, LASEK
During the procedure an ultra thin outer layer of the eye (the epithelium) either is removed completely (PRK) or is floated away from the eye’s surface (LASEK) and laser energy is applied directly to the eye’s surface. Then a bandage contact lens is placed and left to heal.
“The surgery takes a few minutes, is done with the use of local anesthetic drops and the person returns fully to the activities of the after 5-6 days”

Your Surgeon will advise which treatment is most suitable for you during your consultation. If these treatments are unsuitable for you there are many alternatives treatments for vision correction including intraocular lens implants, cataract surgery and contact lenses.
Detailed consultation
Your first step is to book a suitability assessment at PANTHEO Eye Centre. This will be performed by one of our experienced Consultant Eye Surgeons.
The assessment will include measurement of your prescription (refraction), computerized mapping of your cornea and additional technical measurements.
It is helpful to remember to leave your contact lens out for at least 1 week (soft) or 1 month (hard) prior to your assessment, as contact lenses can affect you corneal measurements. We would ask that you bring your old glasses or contact prescriptions with you.
The assessment may last up to an hour. You may have drops put in your eye which may blur your vision so it is advisable not to drive for several hours afterwards.
If you are within our treatment parameters you will be counselled about the risks and benefits of the surgery and have explained what you will experience before, during and after surgery. «The decision needs to be informed and taken WITH the patient and not FOR the patient!»
- The Eye, retina and retinal detachement explained
HOW THE EYE WORKS
Before we talk about what can go wrong, it is important to understand how the eye works when it is working properly.
The eye is like a camera. When you take a picture, the lens in the front of the camera allows light through and focuses that light on the film that covers the back inside wall of the camera. When the light hits the film, a picture is taken.
The eye works in much the same way. The front parts of the eye (the cornea, pupil, and lens) are clear and allow light to pass through. The light also passes through the large space in the centre of the eye called the vitreous cavity. The vitreous cavity is filled with a clear, jelly-like substance called the vitreous or vitreous gel. The light is focused by the cornea and the lens onto a thin layer of tissue called the retina, which covers the back inside wall of the eye. The retina is like the film in a camera. It is the seeing tissue of the eye. When the focused light hits the retina, a picture is taken. Messages about this picture are sent to the brain through the optic nerve. This is how we see.
THE RETINA
The retina has two parts: the peripheral retina and the macula. If you imagine the retina as a circle with a bull’s-eye at the center, the macula is like the bull’s-eye, it is very small. The large area of the retina that surrounds the macula and makes up 95% of the retina is called the peripheral retina.
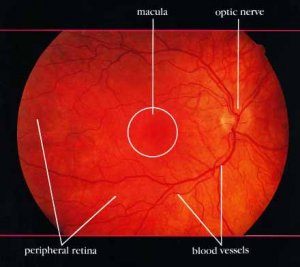
The peripheral retina gives us vision to the side, called ‘peripheral’ vision. It is this part of the retina that is at work when we see something out of the corner of the eye. Because the peripheral retina is not able to see detail clearly, we cannot use the peripheral vision to read, thread a needle, drive, or even recognize a face. If you see someone off to your side, ‘out of the corner of your eye’ you may be able to tell who it is because you recognize the person’s general shape, but you won’t be able to see the expression of the person’s face.
In order to see fine detail, you must look straight ahead, using the macula, the ‘bull’s-eye’ center of the retina. Even though the macula makes up only a small part of the retina, it is one hundred times more sensitive to detail then the peripheral retina. The macula allows you to see tiny detail, read fine print, recognize faces, thread a needle, read the time, see street signs, and drive a car.
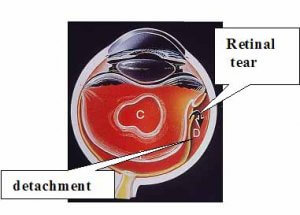
What is retinal detachment?
Retinal detachments often develop in eyes with retinas weakened by a hole or tear. This allows fluid to seep underneath, weakening the attachment so that the retina becomes detached – rather like wallpaper peeling off a damp wall. When detached, the retina cannot compose a clear picture from the incoming rays and vision becomes blurred and dim.
- Retinal Surgery, Important Information and Recovery
You will require surgery to repair your retinal detachment. These are some very important points you need to note:
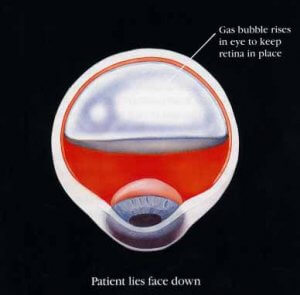
- Usually a special gas is used to push the retina back into place and then laser is applied to ‘weld’ the retina in place. The gas used in detachment surgery will obscure your vision and you may be asked to hold your head in a specific posture to help place the gas against the retinal break.
- The gas is slowly absorbed by you eye and replaced with fluid over a period of about 2 weeks. Sometimes this length of time is not enough for the retina to heal and the detachment returns.
- If this were to happen (5-10% of cases) a second procedure is performed using silicone oil. This behaves in the same way as the gas but cannot be absorbed by your eye and will therefore support the retina for as long as is necessary.
- Although silicone oil has a very high success rate it is only used in very difficult cases because it can be toxic to the eye and needs a procedure in order for it to be removed.
Visual recovery
The degree of visual recovery depends on the extent of the detachment and its duration.
- In general a good proportion of the vision lost will be recovered.
- The vision does not fully recover to its original pre detachment level
- The vision would be totally lost unless surgery is performed
Post operative care
Post-operative medication
You will be given instructions for the use of drops on your first post-operative day. You must use your drops regularly and do not stop them unless you are asked to do so. If you run out buy a new bottle from the chemist.
Cleaning instructions
You must clean you eye for the first ten days using sterilised water only. You can either purchase this from the chemist or boil water and allow it to cool. You must not wet your eye using tap water or shower water.
Dos and don’ts
If gas has been used in your eye you must not go in an aeroplane and avoid high altitude until it has dissolved. Ask your surgeon before you fly
From day one after the surgery you can:
- eat and drink what you like
- read and watch television as much as you like
- return to normal activities as long as you keep your eye clean
- use your old glasses if you find these helpful. If not then don’t use any glasses at all
- wear dark glasses if you want to and if they make you feel more comfortable but they are not necessary
For 15 days you must NOT:
- lift weights greater than 20Kg
- get shower water or tap water into your eye
- go swimming
- get dirt or dust into your eye
It is normal to feel mild discomfort and have mild swelling around your eye for the first few days.
Call the doctor and inform him if:
- you have severe pain
- your eye becomes very swollen
- your vision is deteriorating rather than improving
Questions and answers about retinal detachment
Who is at risk of retinal detachment?
Detachment of the retina is more frequent in middle aged, short sighted people. However, it is quite uncommon and only about one person in ten thousand is affected. It is rare in young adults.
What are the symptoms?
The most common symptom is a shadow spreading across the vision of one eye. You may also experience bright flashes of light and/or showers of dark spots called floaters. These symptoms are never painful. Many people experience flashes or floaters and these are not necessarily a cause for alarm. However, if they are getting severe and seem to be getting worse and you are losing vision, then you should seek medical advice. Prompt treatment can often minimise the damage to your eye.
What is the treatment?
If you get help early, it may only be necessary to have laser or freezing treatment. This is usually performed under a local anaesthetic. Frequently, however, an operation will be needed to repair a hole or put the retina back in place. This is usually done under a general anaesthetic. In 90 – 95 per cent of cases the retina can be repaired with a single operation. The operation does not usually cause much pain, but your eye will be sore and swollen for a few days afterwards. Typically, you will be hospital for a few hours or an overnight stay, depending on your particular condition. We want to reassure you that the surgeon does not take your eye out of its socket to operate on it.
How much vision can I expect after a successful operation?
This depends on how much the retina has detached and for how long. The shadow caused by the detachment will usually disappear when the retina has been put back in place. If your ability to see fine detail has been damaged before the operation, this may not fully recover afterwards.
What happens after the operation?
You will be encouraged to get up and carry on as usual on the day after the operation, although sometimes you will be asked to keep your head in a particular position to help the healing process. Your eye specialist will prescribe eye drops and you will need to use these for a few weeks.
What happens if the detached retina is not put back in place?
Most people will loose all useful vision if no operation is carried out, or if the treatment is unsuccessful. However, further treatment is usually possible if it does not succeed the first time. Occasionally, if the detachment involves the lower portion of the retina, some vision may recover by itself
Can retinal detachment be prevented?
If your family has a history of retinal detachment, or your doctor finds a weakness in your retina, then preventive laser or freezing treatment may be needed. However, in most cases it is not possible to take preventive action. Retinal detachment does not happen as a result of straining your eyes, bending or heavy lifting.
What about my other eye?
If you have had a retinal detachment in one eye, you are at an increased risk of developing one in the other eye. But there is only about a one in ten chance of this happening.